Carotid stenosis (stenosis = narrowing) is the narrowing of carotid arteries in the neck. Carotid arteries carry oxygen-rich blood to a large part of the brain. Gradual narrowing of these arteries causes decrease blood flow to the brain leading to stroke. There are no community based studies describing the incidence and prevalence of carotid artery disease in India. The increasing prevalence of heart disease, diabetes and other risk factors such as obesity only indicates that the incidence of carotid stenosis in India is on the rise. Hence it is important for family doctors and people to be aware of this condition and seek appropriate treatment.
What is carotid stenosis?
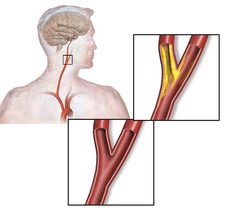
Progressive narrowing of carotid arteries in the neck occurs due to the formation of plaque consisting of fat, cholesterol and calcium. Over time, this plaque gradually prevents adequate amount of blood going to the brain. People with carotid stenosis have an increased risk of having a stroke in one of the three ways:
Every doctor should be aware of this condition and should refer the patient to the appropriate specialist when in doubt. A Stroke Neurologist is the best person to diagnose and manage carotid artery disease initially. Other than a thorough clinical examination, some of the common tests used to diagnose carotid stenosis and plan treatment are

What is carotid stenosis?
Progressive narrowing of carotid arteries in the neck occurs due to the formation of plaque consisting of fat, cholesterol and calcium. Over time, this plaque gradually prevents adequate amount of blood going to the brain. People with carotid stenosis have an increased risk of having a stroke in one of the three ways:
- The plaque may grow larger and larger and may eventually completely block the carotid artery.
- Due to decreased blood flow through the carotid arteries, there is an increased risk of forming blood clots in the carotid artery. These blood clots may go into the brain and block one of the major arteries.
- The plaque may break and block one of the arteries in the brain.
What are the risk factors for carotid stenosis?
- Age
- Smoking
- High blood pressure
- High 'bad' Cholesterol (LDL)
- Diabetes
- Obesity
- Family history of heart disease and stroke
What are the symptoms?
Unfortunately, many people with carotid artery disease do not have symptoms until the late stage and, in many patients stroke may be the first indication of carotid stenosis. Transient ischemic attack (TIA) or 'Warning Stroke' may be another indication of underlying carotid artery disease. Common symptoms of TIA include
Sudden numbness, tingling, weakness, or loss of movement in your face, arm, or leg, especially on only one side of your body.
Sudden vision changes. A special type of TIA is amaurosis fugax. Transient blindness in one eye occurs because debris from a narrowed carotid artery clogs the artery (ophthalmic artery) that supplies blood to the retina of the eye.
Sudden trouble speaking.
Sudden confusion or trouble understanding simple statements.
How is carotid stenosis diagnosed?Sudden problems with walking or balance.
Every doctor should be aware of this condition and should refer the patient to the appropriate specialist when in doubt. A Stroke Neurologist is the best person to diagnose and manage carotid artery disease initially. Other than a thorough clinical examination, some of the common tests used to diagnose carotid stenosis and plan treatment are
- Carotid doppler ultrasound
- CT angiography
- MR angiography
- Digital Subtraction Angiography
How is carotid stenosis treated?
- Lifestyle modification slows the growth of the plaque. This is the most important step in treatment of carotid stenosis
- Depending upon the associated medical conditions, your doctor may prescribe blood thinners such as aspirin, clopidogrel and warfarin. Statins have a major role to play in the medical management of carotid artery disease. High blood pressure, diabetes and heart disease, if present, should be treated appropritely
- Carotid Endarterectomy: In selected patients, surgery may be required to remove the plaque. Surgery involves making an incision in the neck, opening the carotid artery, removing the plaque and sewing the artery back to restore blood flow to the brain

- Carotid angioplasty and stenting: In patients with severe uncontrolled heart disease in whom surgery may carry a high risk, opening the artery from inside and placing a stent by inserting a catheter through the groin may be an option.